Nov. 23, 2021
Pandemic or endemic, testing is first step in preventing serious health outcomes

Test, trace, isolate: three words that after 20 months of the COVID-19 pandemic, we’re all familiar with. Without the first step — testing — the chain reaction of response is slowed, and mitigation of the infection becomes much harder.
Dr. Dylan Pillai, MD, PhD, has been a local leader in COVID-19 testing since March 2020. He was selected as a Peak Scholar in COVID-19 Innovation Excellence for his work developing a highly accurate, ultra-sensitive DNA-based point-of-care COVID-19 test.
The test uses a technique called loop mediated amplification (LAMP) which detects the viral genetic material from a nose or throat swab. LAMP does not require expensive laboratory equipment and the result can be seen without instrumentation.
“DNA-based tests are typically much more sensitive, meaning it can pick up very low-level infections, and not be so prone to false positives,” says Pillai, comparing the LAMP test to rapid antigen tests. “We’re trying to take DNA-based technologies traditionally used in the laboratory to a patient bedside, clinic, pharmacy or airport instead.”
LAMP was used in Alberta’s COVID-19 traveller screening program, which tested over 100,000 individuals arriving at the Calgary airport. “It had immediate impact, immediate benefit,” says Pillai. “This also allowed us to move the technology forward.” With support from Innovate Calgary, a startup company called Illucidx is attempting to further commercialize the technology and boost the Calgary biotechnology ecosystem.
With what they have learned from this large-scale use of LAMP, Pillai and colleagues from the Schulich School of Engineering have designed a smaller, self-contained LAMP testing device called a Biobox. The unit is about the size of a home printer and can produce a COVID-19 test result in about 30 minutes.
In June 2021, they published a paper on the success of the Biobox, demonstrating that it is an excellent option for point-of-care relying on saliva alone. Their goal is to get the technology small enough to fit in someone’s hand, with testing happening within a palm-sized microfluidic cartridge.

An image of Biobox, the self-contained LAMP testing device.
Courtesy of Dylan Pillai
Malaria testing research will benefit from COVID-19 learnings
The volume of research being put into LAMP testing for COVID-19 will continue to have impact beyond the pandemic. Prior to COVID-19, Pillai’s lab was working on point-of-care malaria testing to help address the disease’s impact in affected regions in Africa. That work is now continuing, making use of what Pillai and team have learned from their work on the COVID-19 response.
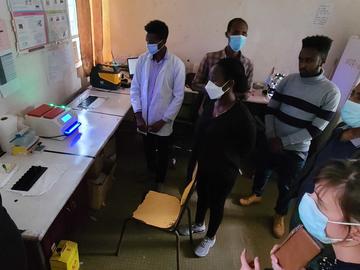
Pillai’s team has launched a malaria testing program in Ethiopia, led by Dr. Claire Kamaliddin, PharmD, PhD, a postdoctoral scholar in Pillai’s lab. The program, funded by Grand Challenges Canada and FIND Geneva, is working with prenatal clinics in Ethiopia to diagnose malaria during pregnancy. Malaria has serious implications during pregnancy if left untreated.
“In endemic areas, people are exposed to malaria during their lives and they slowly build immunity,” Kamaliddin explains. “But during pregnancy, in the placenta a sub-type of parasite has a new environment to thrive. They will stick to the placenta and impair the exchange of nutrients between the parent and the fetus. This restricts the growth of the fetus and you'll have low birth-weight newborns, less than 2.5 kilograms.”
Kamaliddin has organized six testing sites in western Ethiopia, with a goal of enrolling 2,500 pregnant people to participate in the study. They will be tested throughout their pregnancy for malaria using LAMP, and treated when infected by malaria. At the end of the study, Kamaliddin will assess birth outcomes for those who receive treatment after LAMP testing versus those who do not.
These babies are more prone to infections and hindered development later in life, but these outcomes are avoidable with adequate strategies for preventing malaria during pregnancy. The World Health Organization recommends to either treat every pregnant person for the disease, or to test everyone and treat only those infected.
“It’s better to only treat mothers who are infected,” says Kamaliddin. “That’s where LAMP comes in. It is highly precise and can discriminate between different species of the parasite, which require different treatments.”
LAMP is well suited for the challenges of testing for infections in areas with limited access to resources. “It’s portable, it doesn’t need a laboratory, and we’re working to make it inexpensive and easy to use,” says Pillai. “The technology is well suited to the developing world, and the evidence base that Claire develops through this trial will further bolster the value of this type of technology and help us move it forward.
“The work that we’ve been able to do on COVID-19 testing has been a real boost to the activities that we already had underway,” he continues. “Applying what we’ve learned in the COVID-19 pandemic to endemic malaria, and vice versa, shows the importance of translating existing knowledge to new problems. It gives you a head start and can lead to immediate benefit.”
Dylan Pillai is the academic head of the department of Pathology and Laboratory Medicine, and a professor in the departments of Medicine, and Microbiology, Immunology and Infectious Diseases and member of the Snyder Institute for Chronic Diseases and the Alberta Children’s Hospital Research Institute at the Cuming School of Medicine. He is also medical director, south sector, at Alberta Precision Laboratories.
Since 2014, the Peak Scholars program has celebrated the accomplishments of over 200 scholars at the University of Calgary. These are scholars whose academic work in knowledge engagement, entrepreneurship, tech transfer, innovation or collaborative research has resulted in a positive social or economic impact in our communities. Learn more